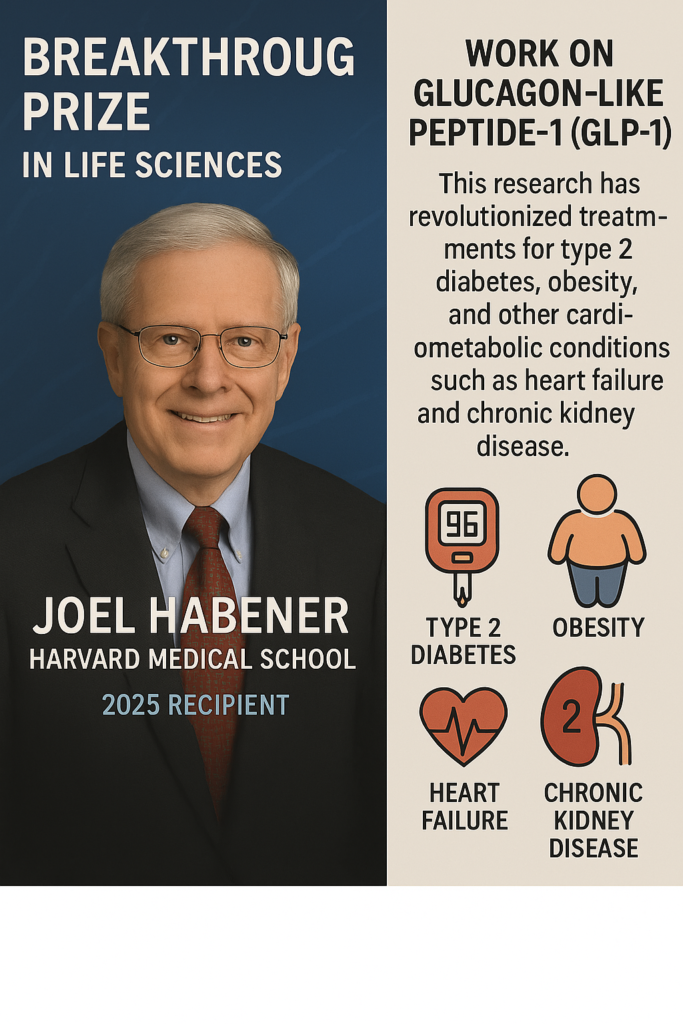
🏆 A Landmark Achievement in Life Sciences
In 2025, Dr. Joel Habener of Harvard Medical School received the prestigious Breakthrough Prize in Life Sciences for his pioneering work on glucagon-like peptide-1 (GLP-1). This hormone has revolutionized the treatment of type 2 diabetes, obesity, and multiple cardiometabolic diseases, such as heart failure and chronic kidney disease.
🔬 What is GLP-1?
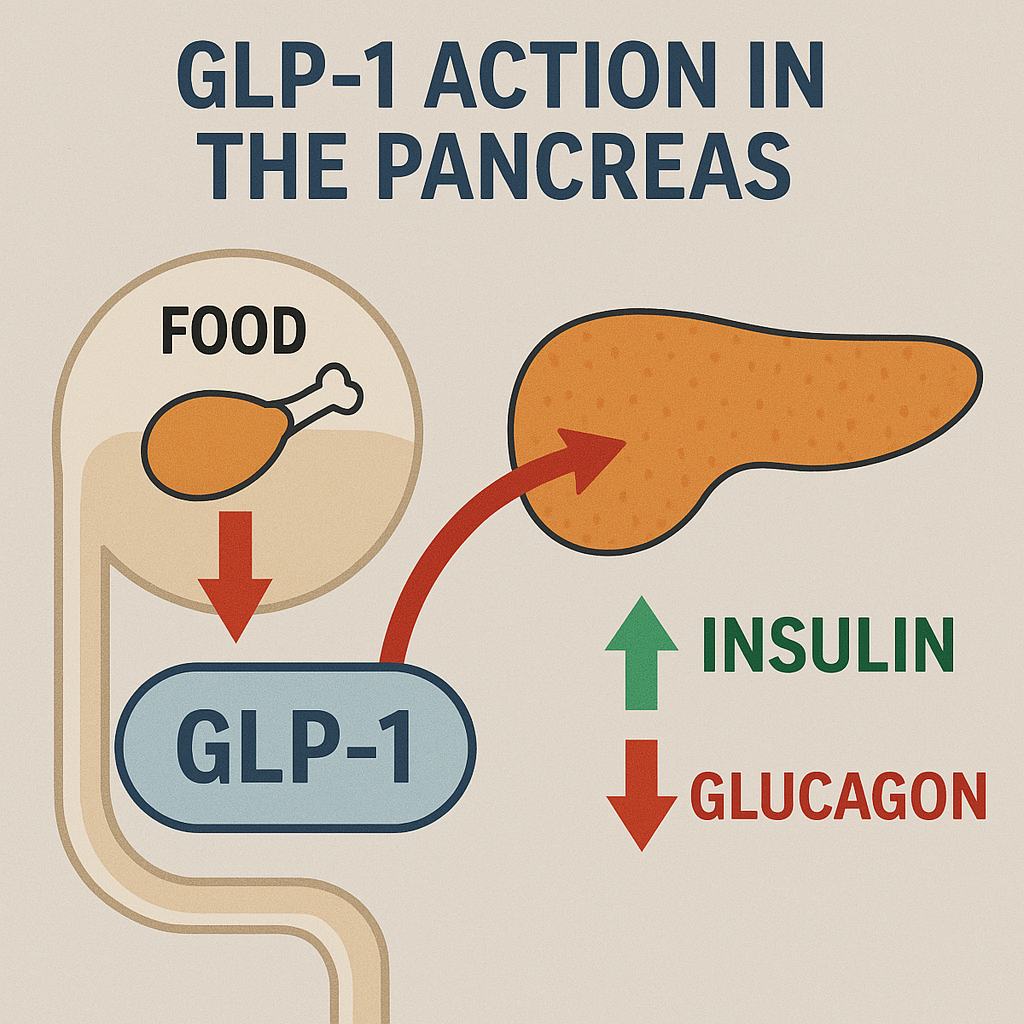
GLP-1 is a naturally occurring hormone in the gut in response to food intake. It plays a key role in:
- Stimulating insulin secretion when blood sugar levels are high
- Suppressing glucagon (a hormone that increases blood sugar)
- Slowing gastric emptying, helping you feel full longer
- Reducing appetite, which aids in weight loss
Dr. Habener’s discovery of how GLP-1 functions has opened the door to new therapeutic drugs known as GLP-1 receptor agonists (e.g., semaglutide, liraglutide), used globally to control:
- 🔵 Type 2 Diabetes
- 🟢 Obesity
- 🟠 Heart Failure
- 🟣 Chronic Kidney Disease
💊 GLP-1 Drugs: A New Era in Medicine
GLP-1 receptor agonists are now blockbuster treatments:
- Semaglutide (branded as Ozempic, Wegovy) has shown exceptional results in blood sugar control, weight reduction, and cardiovascular protection.
- Patients experience 10–15% weight loss — something previously unachievable with medications alone.
- GLP-1 therapies reduce the risk of stroke, heart attack, and kidney damage, improving long-term survival.
👨⚕️ Dr. Joel Habener’s Impact
Dr. Habener’s research, which began in the 1970s, was critical in:
- Identifying the role of proglucagon (the precursor to GLP-1)
- Mapping how GLP-1 is synthesized in the body
- Enabling the development of targeted GLP-1 therapies
His lifelong dedication to endocrine science has helped millions globally.
📊 Infographic Overview
The 2025 Breakthrough Prize celebrates the complementary roles of the five recipients:
- Joel Habener: Habener’s early work identified GLP-1 within the glucagon gene. He demonstrated that GLP-1 is released from gut cells in response to food intake and enhances insulin secretion from pancreatic beta cells. His discoveries suggested that boosting GLP-1 activity could be a therapeutic target for metabolic disorders.
- Svetlana Mojsov: A chemist at The Rockefeller University, Mojsov identified the physiologically active form of GLP-1 (known as GLP-1 (7-37)) and developed innovative methods to synthesize it. Her collaboration with Habener confirmed GLP-1’s insulin-stimulating properties, a critical step toward its clinical application.
- Daniel Drucker: As a postdoctoral fellow in Habener’s lab and later a researcher at the University of Toronto, Drucker expanded the understanding of GLP-1’s broader effects. He showed that it influences not just the pancreas but also the brain, heart, gut, and immune system, revealing its potential beyond diabetes treatment.
- Jens Juul Holst: Working independently at the University of Copenhagen, Holst confirmed GLP-1’s role as an incretin in pigs and humans. He also discovered that it slows gastric emptying and suppresses appetite, key mechanisms that contribute to weight loss.
- Lotte Bjerre Knudsen: At Novo Nordisk, Knudsen translated these biological insights into practical therapies. She led the development of GLP-1-based drugs like liraglutide and semaglutide (marketed as Ozempic and Wegovy), overcoming challenges like the hormone’s short half-life in the body by modifying its structure for longer-lasting effects.
Impact on Type 2 Diabetes and Obesity
The development of GLP-1 receptor agonists—drugs that mimic GLP-1’s actions—has transformed the management of type 2 diabetes and obesity. These conditions affect millions globally: over 460 million people have type 2 diabetes, and more than 1 billion live with obesity. GLP-1 drugs work by:
- Increasing insulin release to lower blood sugar.
- Reducing glucagon secretion to prevent excess glucose production.
- Slowing gastric emptying to enhance satiety and reduce food intake.
- Acting on the brain to suppress appetite.
Clinical trials have shown remarkable results. For example, semaglutide has led to significant weight loss (up to 20% of body weight in some patients) and improved blood sugar control. As of 2024, approximately 12% of U.S. adults have used a GLP-1 medication, reflecting their widespread adoption.
Beyond Diabetes and Obesity: Cardiometabolic Benefits
Recent research has uncovered GLP-1’s broader therapeutic potential. Studies suggest these drugs can:
- Reduce cardiovascular risks: Trials show a 20% lower risk of heart attacks and strokes in patients with obesity and cardiovascular disease.
- Improve heart failure: Patients with obesity and heart failure report better heart function after a year on semaglutide.
- Protect kidney health: GLP-1 therapies reduce the progression of chronic kidney disease in diabetic patients.
- Address fatty liver disease: Emerging evidence indicates benefits for non-alcoholic fatty liver disease, a common obesity-related condition.
These findings have sparked a new field of research into GLP-1’s mechanisms, including its anti-inflammatory effects, which may underlie some of these benefits.
Why This is Matter
The work of Habener and his colleagues exemplifies the power of basic science translating into life-changing therapies. Their discoveries have not only alleviated suffering for millions but also shifted societal perceptions of obesity from a matter of willpower to a treatable chronic illness rooted in biology. As research continues, GLP-1 drugs are being explored for conditions like Alzheimer’s, Parkinson’s, and addiction, hinting at an even broader impact in the future.
Leave a Reply